US and UK Researchers Simultaneously Develop New Tests to Detect Prostate Cancer
Though still in trials, early results show tests may be more accurate than traditional clinical laboratory tests for detecting prostate cancer
Within weeks of each other, different research teams in the US and UK published findings of their respective efforts to develop a better, more accurate clinical laboratory prostate cancer test. With cancer being a leading cause of death among men—second only to heart disease according to the Centers for Disease Control and Prevention (CDC)—new diagnostics to identify prostate cancer would be a boon to precision medicine treatments for the deadly disease and could save many lives.
Researchers at the University of East Anglia (UEA) in Norwich, England, were working to improve the accuracy of the widely-used and accepted prostate-specific antigen (PSA) test. By contrast, researchers at Cedars-Sinai Cancer in Los Angeles, pursued a new liquid biopsy approach to identifying prostate cancer that uses nanotechnology.
Thus, these are two different pathways toward the goal of achieving earlier, more accurate diagnosis of prostate cancer, the holy grail of prostate cancer diagnosis.

“There is currently no single test for prostate cancer, but PSA blood tests are among the most used, alongside physical examinations, MRI scans, and biopsies,” said Dmitry Pshezhetskiy, PhD (above), Professorial Research Fellow at University of East Anglia and one of the authors of the UEA study. “However, PSA blood tests are not routinely used to screen for prostate cancer, as results can be unreliable. Only about a quarter of people who have a prostate biopsy due to an elevated PSA level are found to have prostate cancer. There has therefore been a drive to create a new blood test with greater accuracy.” With the completion of the US and UK studies, clinical laboratories may soon have a new diagnostic test for prostate cancer. (Photo copyright: University of East Anglia.)
East Anglia’s Research into a More Accurate Blood Test
Scientists at the University of East Anglia (UEA) worked with researchers from Imperial College in London, Imperial College NHS Trust, and Oxford BioDynamics to develop a new precision medicine blood test that can detect prostate cancer with greater accuracy than current methods.
The epigenetic blood test they developed, called Prostate Screening EpiSwitch (PSE), can identify cancer-specific chromosome conformations in blood samples. The test works in tandem with the standard prostate-specific antigen (PSA) blood test to diagnose prostate cancer, according to an Oxford BioDynamics press release.
The researchers evaluated their test in a pilot study involving 147 patients. They found their testing method had a 94% accuracy rate, which is higher than that of PSA testing alone. They discovered their test significantly improved the overall detection of prostate cancer in men who are at risk for the disease.
“When tested in the context of screening a population at risk, the PSE test yields a rapid and minimally invasive prostate cancer diagnosis with impressive performance,” Dmitry Pshezhetskiy, PhD, Professorial Research Fellow at UEA and one of the authors of the study told Science Daily. “This suggests a real benefit for both diagnostic and screening purposes.”
The UK scientists hope their test can eventually be used in everyday clinical practice as there is a need for a highly accurate method for prostate cancer screening that does not subject patients to unnecessary, costly, invasive procedures.
The UEA researchers published their findings in the peer-reviewed journal Cancers, titled, “Circulating Chromosome Conformation Signatures Significantly Enhance PSA Positive Predicting Value and Overall Accuracy for Prostate Cancer Detection.”
Cedars-Sinai’s Research into Nanotechnology Cancer Testing
Researchers from Cedars-Sinai Cancer took a different approach to diagnosing prostate cancer by developing a nanotechnology-based liquid biopsy test that detects the disease even in microscopic amounts.
Their test isolates and identifies extracellular vesicles (EVs) from blood samples. EVs are microscopic non-reproducing protein and genetic material shed by all cells. Cedars-Sinai’s EV Digital Scoring Assay accurately extracts EVs from blood and analyzes them faster than similar currently available tests.
“This research will revolutionize the liquid biopsy in prostate cancer,” said oncologist Edwin Posadas, MD, Medical Director of the Urologic Oncology Program and co-director of the Experimental Therapeutics Program in Cedars-Sinai Cancer in a press release. “The test is fast, minimally invasive and cost-effective, and opens up a new suite of tools that will help us optimize treatment and quality of life for prostate cancer patients.”
The researchers tested blood samples from 40 patients with prostate cancer. They found that their EV test could distinguish between cancer localized to the prostate and cancer that has spread to other parts of the body.
Microscopic cancer deposits, called micrometastases, are not always detectable, even with advanced imaging methods. When these deposits spread outside the prostate area, focused radiation cannot prevent further progression of the disease. Thus, the ability to identify cancer by locale within the body could lead to new precision medicine treatments for the illness.
“[The EV Digital Scoring Assay] would allow many patients to avoid the potential harms of radiation that isn’t targeting their disease, and instead receive systemic therapy that could slow disease progression,” Posadas explained.
The Cedars-Sinai researchers published their findings in Nano Today, titled, “Prostate Cancer Extracellular Vesicle Digital Scoring Assay: A Rapid Noninvasive Approach for Quantification of Disease-relevant mRNAs.”
Other Clinical Laboratory Tests for Prostate Cancer Under Development
According to the American Cancer Society, the number of prostate cancer cases is increasing. One out of eight men will be diagnosed with the illness during his lifetime. Thus, developers have been working on clinical laboratory tests to accurately detect the disease and save lives for some time.
In “University of East Anglia Researchers Develop Non-Invasive Prostate Cancer Urine Test,” Dark Daily reported on a urine test also developed by scientists at the University of East Anglia that clinical laboratories can use to not only accurately diagnose prostate cancer but also determine whether it is an aggressive form of the disease.
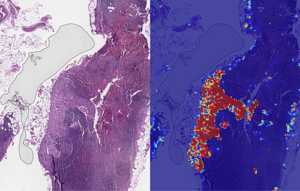
And in “UPMC Researchers Develop Artificial Intelligence Algorithm That Detects Prostate Cancer with ‘Near Perfect Accuracy’ in Effort to Improve How Pathologists Diagnose Cancer ,” we outlined how researchers at the University of Pittsburgh Medical Center (UPMC) working with Ibex Medical Analytics in Israel had developed an artificial intelligence (AI) algorithm for digital pathology that can accurately diagnose prostate cancer. In the initial study, the algorithm—dubbed the Galen Prostate AI platform—accurately detected prostate cancer with 98% sensitivity and 97% specificity.
More research and clinical trials are needed before the new US and UK prostate cancer testing methods will be ready to be used in clinical settings. But it’s clear that ongoing research may soon produce new clinical laboratory tests and diagnostics for prostate cancer that will steer treatment options and allow for better patient outcomes.
—JP Schlingman
Related Information:
The New Prostate Cancer Blood Test with 94 Percent Accuracy
Invention: A Blood Test to Unlock Prostate Cancer Mysteries
Could a Urine Test Detect Pancreatic and Prostate Cancer? Study Shows 99% Success Rate
University of East Anglia Researchers Develop Non-Invasive Prostate Cancer Urine Test