Clinical laboratory and pathology groups that support ambulatory and virtual care, and urgent care and retail clinics may experience growth
Global management consulting company McKinsey and Company’s report, “The Great Acceleration In Healthcare: Six Trends to Heed,” identifies six trends in healthcare that are accelerating due to the global COVID-19 pandemic.
Clinical laboratory managers and pathology practice administrators should consider how these trends may affect their business and patients when planning for the future.
1: Healthcare Reform
McKinsey identified three areas where the coronavirus pandemic may impact healthcare reform:
- “COVID-19-era waivers that could become permanent.
- “Actions that may be taken to strengthen the healthcare system to deal with pandemics.
- “Reforms to address the COVID-19-induced crisis.”
McKinsey reports that “the Centers for Medicare and Medicaid Services has introduced more than 190 waivers since the beginning of March 2020.” These waivers can affect all aspects of healthcare, from clinical practice to reimbursement. Some of them, according to McKinsey, are “only relevant during the crisis (for example, the waiver of intensive care unit death reporting). A retrospective assessment of others (for example, expansion of telehealth access) could reveal beneficial innovation worth preserving.”
Several areas that McKinsey says are clearly ripe for reform include improving the resiliency of the healthcare system and the way the system is funded.
Public sector budgets are generally kept strictly separate, each with its own rules and policies that dictate operations. But in his article, “After COVID-19—Thinking Differently About Running the Health Care System,” published in JAMA Health Network, Stuart M. Butler, PhD, Senior Fellow in Economic Studies at the Brookings Institution, wrote, “The intensity of the COVID-19 pandemic … is forcing jurisdictions all across the country to find ways to be nimble so that multiple agencies can work together.”
Thus, McKinsey recommends, “Given the substantial shifts in relative market positioning among industry players that prior reforms have created, leaders would do well to plan ahead now.”
2: Better Access to Healthcare Services
Some people who develop COVID-19 are at far greater risk of hospitalization and death than others, including those who have:
- Chronic health conditions, including obesity.
- Mental and behavioral health challenges, such as substance abuse.
- Unmet social needs, such as food or housing insecurity.
- Poor access to healthcare.
McKinsey wrote that these “intersecting health and social conditions,” combined with certain races that have higher risk for severe complications, including Black, Indian, and Hispanic/Latino Americans, “correlated with poorer health outcomes.”
Value-based healthcare, telehealth, and greater attention to the social determinants of health may help address some of these issues, McKinsey notes, but the pandemic has shined a spotlight on how lack of care increases risk for certain populations during a public health crisis.
3: Era of Exponential Improvement Unleashed
Some of the trends that appear to be accelerating as a result of the pandemic are good news. McKinsey cites several benefits, including:
- Improved understanding of patients.
- Delivery of more convenient and individualized care.
- $350-$410 billion in annual revenue by 2025.
Through telehealth and other types of virtual care enabled by digital technology, “intuitive healthcare ecosystems” may arise and offer a more integrated experience for patients and their caregivers, McKinsey notes.
“While the pace of change in healthcare has lagged other industries in the past, potential for rapid improvement may accelerate due to COVID-19. An example is the exponential uptake of digitally enabled, virtual care,” McKinsey wrote. “Our analysis … showed that health systems, primary care, and behavioral health practices are reporting increases of more than 50–175 times in telehealth visits, and the potential market size for virtual care could reach around $250 billion.”

4: The Big Squeeze
The pandemic has caused an enormous outflow of cash from the healthcare system, and some experts don’t expect an injection of funding until 2022. “This outflow is expected to be primarily driven by coverage shifts out of employer-sponsored insurance and possible coverage reductions by employers as well as Medicaid rate pressures from states,” McKinsey states.
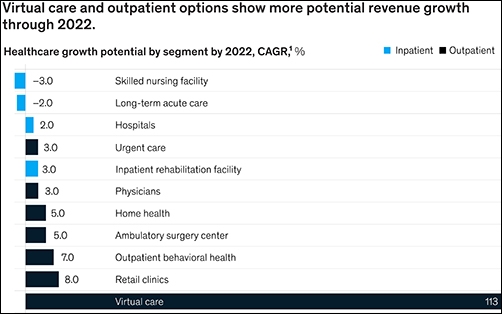
“We estimate that COVID-19 could depress healthcare industry earnings by between $35 billion and $75 billion compared with baseline expectations,” McKinsey predicted, adding, “Select high-growth segments will remain attractive (for example, virtual care, home health, software and platforms, specialty pharmacy) and will disproportionally drive growth. These high-growth areas are expected to increase more than 10% over the next five years, while other segments may stagnate or decline altogether.”
5: Fragmented, Integrated, Consolidated Care Delivery
McKinsey says, “The shift of care out of hospitals is not new but has been accelerated by COVID-19.” Rather than the hospital being the center of care delivery, patients are increasingly choosing to receive care at a range of sites across many healthcare ecosystems that are connected digitally and through analytics.
Early in the course of the pandemic, visits to ambulatory care facilities dropped nearly 60% by early April. But by mid-May, those visits were beginning to rebound.
In, “The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges,” the Commonwealth Fund reported that “the relative decline in visits remains largest among surgical and procedural specialties and pediatrics” but is “smaller in other specialties, such as adult primary care and behavioral health.”
6: Adoption of Next-Generation Managed Care Is Accelerating
How will COVID-19 affect the managed care industry? McKinsey says the “next generation” of managed care might use Medicare Advantage as a model.
“Payers pursuing the next generation of managed care model (through deep integration with care delivery) demonstrate better financial performance, capturing an additional 50 basis points of earnings before interest, taxes, depreciation, and amortization above expectation,” McKinsey noted, adding, “Employers and payers could consider fundamentally rethinking how employer-sponsored health coverage is structured. Learning from Medicare Advantage could provide inspiration for such a reimagination.”
What Should Clinical Laboratory Managers Do?
The McKinsey article concludes by stating, “While the challenges are numerous, leaders who seize the mindset that “disruptive change provides an opportunity to separate yourself from the pack” will build organizations meaningfully stronger than the ones they ran going into the crisis.”
The McKinsey article authors recommend that healthcare organizations take several proactive steps, including:
- Launch a plan-ahead team.
- Question your role and your future business model.
- Prepare to transform your business.
- Reimagine your organization to make faster decisions.
- Take action to drive health equity.
Though the McKinsey and Company article covered healthcare in general, many of the authors’ observations and recommendations can apply to clinical laboratories and pathology groups as well and may be valuable in future planning.
—Dava Stewart
Related Information:
The Great Acceleration in Healthcare: 6 Trends to Heed:
After COVID-19—Thinking Differently About Running the Health Care System:
The Next Wave of Healthcare Innovation: The Evolution of Ecosystems
The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges





It all comes down to health equity. The industry needs more people who could think about improving the system rather than becoming just a cog in the wheel.