UCF Researchers Develop an Optical Sensor That Identifies Viruses in Blood Samples in Seconds with 95% Accuracy
New nanotechnology device is significantly faster than typical rapid detection clinical laboratory tests and can be manufactured to identify not just COVID-19 at point of care, but other viruses as well
Researchers at the University of Central Florida (UCF) announced the development of an optical sensor that uses nanotechnology to identify viruses in blood samples in seconds with an impressive 95% accuracy. This breakthrough underscores the value of continued research into technologies that create novel diagnostic tests which offer increased accuracy, faster speed to answer, and lower cost than currently available clinical laboratory testing methods.
The innovative UCF device uses nanoscale patterns of gold that reflect the signature of a virus from a blood sample. UCF researchers claim the device can determine if an individual has a specific virus with a 95% accuracy rate. Different viruses can be identified by using their DNA sequences to selectively target each virus.
According to a UCF Today article, the University of Central Florida research team’s device closely matches the accuracy of widely-used polymerase chain reaction (PCR) tests. Additionally, the UCF device provides nearly instantaneous results and has an accuracy rate that’s a marked improvement over typical rapid antigen detection tests (RADT).
However, both the Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) have cautioned that rapid antigen tests could produce inaccurate test results if viral loads are low or test instructions are not followed properly.
The UCF researchers published their findings in the journal Nano Letters, titled, “DNA-Modified Plasmonic Sensor for the Direct Detection of Virus Biomarkers from the Blood.”
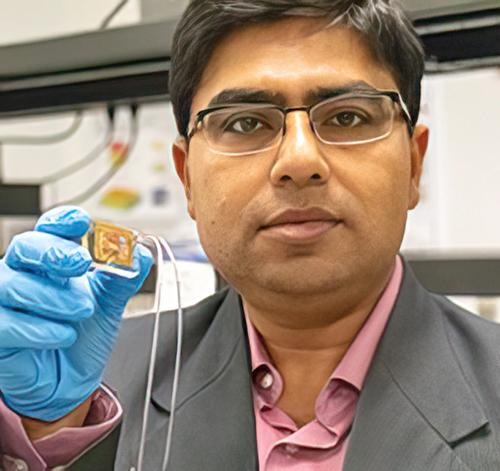
Genetic Virus Detection on a Chip
“The sensitive optical sensor, along with the rapid fabrication approach used in this work, promises the translation of this promising technology to any virus detection, including COVID-19 and its mutations, with high degree of specificity and accuracy,” Debashis Chanda, PhD, told UCF Today. Chanda is professor of physics at the NanoScience Technology Center at UCF and one of the authors of the study. “Here, we demonstrated a credible technique which combines PCR-like genetic coding and optics on a chip for accurate virus detection directly from blood.”
The team tested their device using samples of the Dengue virus that causes Dengue fever, a tropical disease spread by mosquitoes. The device can detect viruses directly from blood samples without the need for sample preparation or purification. This feature enables the testing to be timely and precise, which is critical for early detection and treatment of viruses. The chip’s capability also can help reduce the spread of viruses.
No Pre-processing or Sample Preparation Needed for Multi-virus Testing
The scientists confirmed their device’s effectiveness with multiple tests using varying virus concentration levels and solution environments, including environments with the presence of non-target virus biomarkers.
“A vast majority of biosensors demonstrations in the literature utilize buffer solutions as the test matrix to contain the target analyte,” Chanda told UCF Today. “However, these approaches are not practical in real-life applications because complex biological fluids, such as blood, containing the target biomarkers are the main source for sensing and at the same time the main source of protein fouling leading to sensor failure.”
The researchers believe their device can be easily adapted to detect other viruses and are optimistic about the future of the technology.
“Although there have been previous optical biosensing demonstrations in human serum, they still require off-line complex and dedicated sample preparation performed by skilled personnel—a commodity not available in typical point-of-care applications,” said Abraham Vazquez-Guardado, PhD, a Postdoctoral Fellow at Northwestern University who worked on the study, in the UCS Today article. “This work demonstrated for the first time an integrated device which separated plasma from the blood and detects the target virus without any pre-processing with potential for near future practical usages.”
More research and additional studies are needed to develop the University of Central Florida scientists’ technology and prove its efficacy. However, should the new chip prove viable for point-of-care testing, it would give clinical laboratories and microbiologists an ability to test blood samples without any advanced preparation. Combined with the claims for the device’s remarkable accuracy, that could be a boon not only for COVID-19 testing, but for testing other types of viruses as well.
—JP Schlingman
Related Information:
UCF Researchers Develop Rapid, Highly Accurate Test to Detect Viruses like COVID-19
Researchers Develop Rapid, Highly Accurate Virus Detection Test
DNA-Modified Plasmonic Sensor for the Direct Detection of Virus Biomarkers from the Blood



