Where Did all the Antibodies Go? Emory University’s Vaccine Center Studies Bone Marrow to Find Out Why Influenza Vaccines are Short-Lived
Pathologists and clinical laboratory scientists know that influenza vaccines typically produce short-lived protection and researchers have new clues as to why this is true
With so much interest in development of a COVID-19 vaccine, findings by researchers at Atlanta’s Emory Vaccine Center into why the vaccine for influenza (Flu) is so short-lived offer a new window on how the body’s immune system responds to invading viruses and what happens to the immunity over time.
Because the autumn influenza season is just weeks away, these insights into the body’s immune response to influenza will be of interest to clinical laboratories that provide testing for influenza, as well as SARS-CoV-2, the coronavirus that causes COVID-19.
Clinical laboratory managers recognize that an influenza vaccine is an annual imperative for people—especially the elderly and those with existing comorbidities—and medical laboratory tests are typically used to diagnose the illness and identify which strains of viruses are present. The flu vaccine is even more important amid the COVID-19 pandemic, infectious disease authorities say.
The scientists at the Emory Vaccine Center published their findings in the journal Science.
How Does Influenza Differ from Other Viruses?
Vaccines for some viruses, such as Hepatitis A, Hepatitis B, and the human papillomavirus, may be taken only one time, but the immunity can last a lifetime.
Not so with influenza vaccines. The immunity they impart generally only lasts for a single flu season and are “lost within one year,” the Emory study notes.
As Genetic Engineering and Biotechnology News (GEN) explains, the influenza genome has eight RNA segments which can change as the virus enters a cell. This antigenic shift creates new influenza strains that require updated vaccines, GEN noted.
However, the Emory researchers stated that “The fact that a small number did persist over one year raises prospects that the longevity of flu vaccines can be improved and provides key information for the development of universal vaccines against influenza.”
Bone Marrow Has Major Role in Producing New Flu Antibodies
The Emory study focused on the influenza vaccine’s role in how it affects the immune system and what needs to change to create a longer-lasting influenza vaccine. “Our results suggest that most bone marrow plasma cells (BMPC) generated by influenza vaccination in adults are short-lived. Designing strategies to enhance their persistence will be key,” the Emory researchers wrote in Science.
The scientists analyzed bone marrow from 53 healthy volunteers (age 20 to 45). An Emory news release states that bone marrow is the “home base for immune cells producing antibodies.”
Besides the bone marrow, the researchers also examined blood samples from the volunteers, all of which was collected between 2009 and 2018:
- before influenza vaccination,
- one month after influenza vaccination, and
- one year post vaccination.
Through DNA sequencing the samples, the Emory researchers found the number of flu-specific cells increased from 0.8% to 1.9% after one month. They concluded that an annual vaccine does increase antibody-producing cells for influenza in bone marrow.
However, in follow-up visits one year after vaccination, they found that the number of cells present in the volunteers had fallen back to the starting point.
“Specific cells produced by the vaccine … produced unique antibodies that can be identified using sequencing techniques,” Carl Davis, PhD, postdoctoral fellow in the Rafi Ahmed Laboratory at Emory and first author of the paper, said in the news release, adding, “We could see that these new antibodies expanded in the bone marrow one month after vaccination and then contracted after one year.”
He continued, “On the other hand, antibodies against influenza that were in the bone marrow before the vaccine was given stayed at a constant level over one year.”
Vaccine Adjuvants Help Boost Immunity
A vaccine additive called an adjuvant could be the answer to extending the power of influenza vaccines, the Emory scientists noted.
“Just getting to the bone marrow is not enough. A plasma cell has to find a niche within the bone marrow and establish itself there and undergo gene expression and metabolism changes that promote longevity,” Rafi Ahmed, PhD, Director of the Emory Vaccine Center, said in the news release.
Adjuvants could boost BMPC, because they act as “irritants” to beef up immune response, an article in Science titled, “Why Flu Vaccines Don’t Protect People for Long,” explained.
“It’s totally crazy (that the most commonly used influenza vaccines don’t include an adjuvant), Ahmed told Science. “I’m hoping that things will change in the influenza vaccine world, and 10 years from now, you will not be getting any nonadjuvanted vaccines.”
Are Adjuvants the Answer for COVID-19 Vaccines?
According to USA Today, about 20-million “essential” workers will likely be the first to receive the new COVID-19 vaccine and participate in check-in text messages with the Centers for Disease Control and Prevention (CDC) by the end of 2020.
In its COVID-19 vaccine testing, Novavax, a late-state biotechnology company, suggests that “an adjuvant is critical to its vaccine working well,” National Public Radio (NPR) reported in “The Special Sauce That Makes Some Vaccines Work.” However, vaccine developers may be reluctant to share their adjuvant research.
“Adjuvants end up being very proprietary. It’s kind of the secret sauce on how to make your protein vaccine work,” Barney Graham, MD, PhD, Deputy Director, Vaccine Research Center, National Institute of Allergy and Infectious Diseases, told NPR.
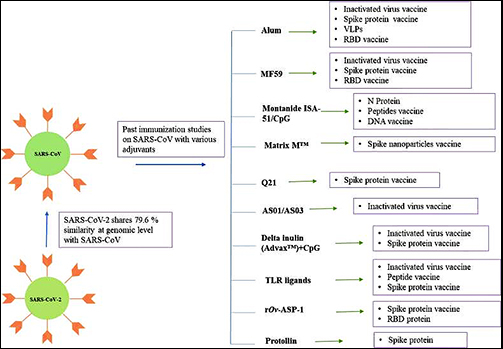
Still, a study published in Immunopharmacology revealed potential adjuvants for the COVID-19 vaccine based on vaccine studies of other coronaviruses. While there are many adjuvants available, not all have safety track records that can be leveraged to gain clearance from regulatory bodies, the researchers pointed out. But some do.
“CpG 1018, MF59, and AS03 are already approved for human vaccine and their inclusion may expedite the vaccine development process. Further, Protollin has shown promising results in pre-clinical studies,” the authors wrote.
Clinical laboratories that provide influenza testing will want to follow these types of research studies. Findings on immunity will affect development of vaccines that medical labs provide—including for COVID-19.
—Donna Marie Pocius
Related Information:
Why Flu Vaccine Immunity is Short-Lived
Influenza Vaccine-induced Human Bone Marrow Plasma Cells Decline Within a Year After Vaccination
Seasonal Flu Vaccinations Don’t “Stick” Long-Term in Bone Marrow
Why Flu Vaccines Don’t Protect People for Long
First COVID-19 Vaccine Recipients Get Daily CDC Check Texts
Administration Announces $200 Million From CDC to Jurisdictions for COVID-19 Vaccine Preparedness
All You Wanted to Know About the Coronavirus Vaccine Science but Were Afraid to Ask




