US Hospitals Continue to Be Squeezed by Shortage of Nurses, Rising Salaries
It is more than a shortage of nurses, as most clinical laboratories report the same shortages of medical technologists and increased labor costs
Just as hospital-based clinical laboratories are unable to hire and retain adequate numbers of medical technologists (MTs) and clinical laboratory scientists (CLSs), the nursing shortage is also acute. Compounding the challenge of staffing nurses is the rapid rise in the salaries of nurses because hospitals need nurses to keep their emergency departments, operating rooms, and other services open and treating patients while also generating revenue.
The nursing shortage has been blamed on burnout due to the COVID-19 pandemic, but nurses also report consistently deteriorating conditions and say they feel undervalued and under-appreciated, according to Michigan Advance, which recently covered an averted strike by nurses at 118-bed acute care McLaren Central Hospital in Mt. Pleasant and 97-bed teaching hospital MyMichigan Medical Center Alma, both in Central Michigan.
“Nurses are leaving the bedside because the conditions that hospital corporations are creating are unbearable. The more nurses leave, the worse it becomes. This was a problem before the pandemic, and the situation has only deteriorated over the last three years,” said Jamie Brown, RN, President of the Michigan Nurses Association (MNA) and a critical care nurse at Ascension Borgess Hospital in Kalamazoo, Michigan Advance reported.

“The staffing crisis will never be adequately addressed until working conditions at hospitals are improved,” said Jamie Brown, RN (above), President of the Michigan Nurses Association in a press release. Brown’s statement correlates with claims by laboratory technicians about working conditions in clinical laboratories all over the country that are experiencing similar shortages of critical staff. (Photo copyright: Michigan Nurses Association.)
Nurse Understaffing Dangerous to Patients
In the lead up to the Michigan nurses’ strike, NPR reported on a poll conducted by market research firm Emma White Research LLC on behalf of the MNA that found 42% of nurses surveyed claimed “they know of a patient death due to nurses being assigned too many patients.” The same poll in 2016 found only 22% of nurses making the same claim.
And yet, according to an MNA news release, “There is no law that sets safe RN-to-patient ratios in hospitals, leading to RNs having too many patients at one time too often. This puts patients in danger and drives nurses out of the profession.”
Other survey findings noted in the Emma White Research memo to NPR include:
- Seven in 10 RNs working in direct care say they are assigned an unsafe patient load in half or more of their shifts.
- Over nine in 10 RNs say requiring nurses to care for too many patients at once is affecting the quality of patient care.
- Requiring set nurse-to-patient ratios could also make a difference in retention and in returning qualified nurses to the field.
According to NPR, “Nurses across the state say dangerous levels of understaffing are becoming the norm, even though hospitals are no longer overwhelmed by COVID-19 patients.”
Thus, nursing organizations in Michigan, and the legislators who support change, have proposed the Safe Patient Care Act which sets out to “to increase patient safety in Michigan hospitals by establishing minimum nurse staffing levels, limiting mandatory overtime for RNs, and adding transparency,” according to an MNA news release.
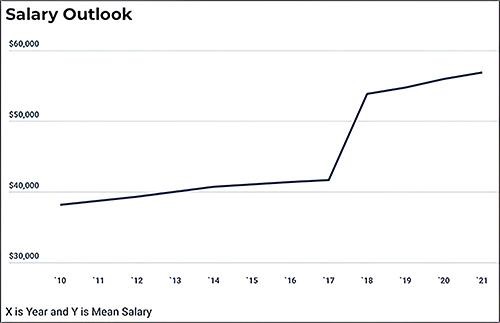
Huge Increase in Nursing Costs
Another pressure on hospitals is the rise in the cost of replacing nurses with temporary or travel nurses to maintain adequate staffing levels.
In “Hospital Temporary Labor Costs: a Staggering $1.52 Billion in FY2022,” the Massachusetts Health and Hospital Association noted that “To fill gaps in staffing, hospitals hire registered nurses and other staff through ‘traveler’ agencies. Traveler workers, especially RNs in high demand, command higher hourly wages—at least two or three times more than what an on-staff clinician would earn. Many often receive signing bonuses. In Fiscal Year 2019, [Massachusetts] hospitals spent $204 million on temporary staff. In FY2022, they spent $1.52 billion—a 610% increase. According to the MHA survey, approximately 77% of the $1.52 billion went to hiring temporary RNs.”
It’s likely this same scenario is playing out in hospitals all across America.
Are Nursing Strikes a Symptom of a Larger Healthcare Problem?
In “Nurses on Strike Are Just the Tip of the Iceberg. The Care Worker Shortage Is About to Touch Every Corner of the US Economy,” Fortune reported that nationally the US is facing a shortage of more than 200,000 nurses.
“But the problem is much bigger,” Fortune wrote. “Care workers—physicians, home health aides, early childhood care workers, physician assistants, and more—face critical challenges as a result of America’s immense care gap that may soon touch every corner of the American economy.”
Clinical laboratories are experiencing the same shortages of critical staff due in large part to the same workplace issues affecting nurses. Dark Daily covered this growing crisis in several ebriefings.
In “Forbes Senior Contributor Covers Reasons for Growing Staff Shortages at Medical Laboratories and Possible Solutions,” we covered an article written by infectious disease expert Judy Stone, MD, in which she noted that factors contributing to the shortage of medical technologists and other clinical laboratory scientists include limited training programs in clinical laboratory science, pay disparity, and staff retention.
We also covered in that ebrief how the so-called “Great Resignation” caused by the COVID-19 pandemic has had a severe impact on clinical laboratory staffs, creating shortages of pathologists as well as of medical technologists, medical laboratory technicians, and other lab scientists who are vital to the nation’s network of clinical laboratories.
And in “Clinical Laboratory Technician Shares Personal Journey and Experience with Burnout During the COVID-19 Pandemic,” we reported on the personal story of Suzanna Bator, a former laboratory technician with the Cleveland Clinic and with MetroHealth System in Cleveland, Ohio. Bator shared her experiences in an essay for Daily Nurse that took a personalized, human look at the strain clinical laboratory technicians were put under during the SARS-CoV-2 pandemic. Her story presents the quandary of how to keep these critical frontline healthcare workers from experiencing burnout and leaving the field.
Did Experts See the Shortages Coming?
Hospitals across the United States—and in the UK, according to Reuters—are facing worker strikes, staff shortages, rising costs, and uncertainty about the future. Just like clinical laboratories and other segments of the healthcare industry, worker burnout and exhaustion in the wake of the COVID-19 pandemic are being cited as culprits for these woes.
But was it predictable and could it have been avoided?
“One of the big things to clear up for the public is that … we saw the writing on the wall that vacancies were going to be a problem for us, before the pandemic hit our shores,” Christopher Friese, PhD, professor of Nursing and Health Management Policy at the University of Michigan (UM), told NPR. Friese is also Director of the Center for Improving Patient and Population Health at UM.
Effects of the COVID-19 pandemic, and staffing shortages exasperated by it, will be felt by clinical laboratories, pathology groups, and the healthcare industry in general for years to come. Creative solutions must be employed to avoid more staff shortages and increase employee retention and recruitment.
—Ashley Croce
Related Information:
Amid Burnout and Exhaustion, Nurses at Two Mid-Michigan Hospitals OK New Contracts
‘Everyone Is Exhausted and Burned Out’: McLaren Central Nurses Authorize Potential Strike
New Poll Shows a Nurse-to-Patient Ratio Law Could Be Key to Addressing Staffing Crisis
42% of Michigan Nurses Say High Patient Load Led to Deaths
Michigan Nurses Report More Patients Dying Due to Understaffing, Poll Finds
COVID-19’s Impact on Nursing Shortages, the Rise of Travel Nurses, and Price Gouging
Survey of Registered Nurses Living or Working in Michigan
This Nursing Shortage Requires Innovative Solutions
Workers Stage Largest Strike in History of Britain’s Health Service
Nursing Shortage by State: Which US States Need Nurses the Most and Which Ones Will Have Too Many?