This is the first of a three-part series on revenue cycle management for molecular testing laboratories and pathology practices, produced in collaboration with XiFin, Inc.
Setting Your Organization Up for Success: Maximizing Revenue for Molecular Diagnostics and Pathology Testing Starts Well Before Billing
What progressive revenue cycle management technology reveals about revenue levers, test clearances, and strategic planning for molecular and pathology testing.
CFOs and other leaders of molecular testing laboratories and pathology groups need to raise their awareness of the most vulnerable aspects of revenue. To this end, this article outlines three specific areas of potential revenue cycle management (RCM) improvement so molecular diagnostic and pathology organizations can better identify and adapt to localized market dynamics and individual patient needs.
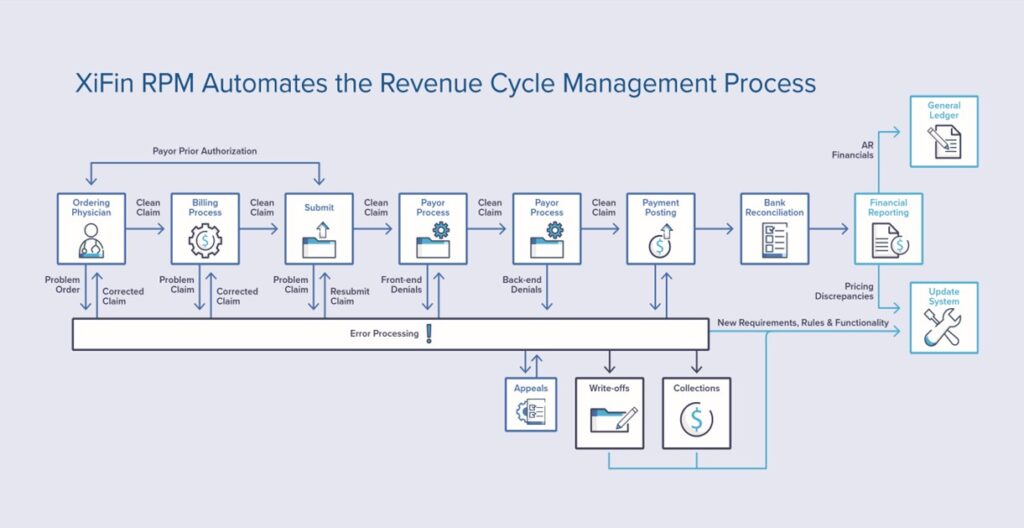
“Many people look at RCM as just billing or getting a clean billing process, but laboratory testing is getting more complex; consequently, reimbursement is getting more complicated, and continually changing payer policies are also making it more challenging for labs to keep up. It is important for business executives, revenue cycle leaders, and CFOs to look more broadly at the revenue cycle,” explained Clarisa Blattner, XiFin Senior Director of Revenue and Payor Optimization. XiFin recommends lab and pathology leaders consider revenue cycle within the broader context of the patient journey, which generally includes, among other things, three key revenue-impacting patient engagement stages.
The first of the three stages, patient access and financial clearance, begins when patient demographics and insurance information are captured. Following demographics and insurance details is a determination of benefits coverage and verification of eligibility. Financial information on any required copay and deductibles are determined, and pre-payment is collected. Finally, the patient receives a financial responsibility estimate for any out-of-pocket expenses.
In stage 2, clinical/medical clearance requires ordering physician engagement to address medical necessity questions and obtain supporting documentation. Clinical assessment and diagnostic testing are conducted. The encounter document is completed. Results are shared via secure, seamless, connected communication between the ordering physician’s office, the lab of the diagnostic provider, and the patient. Finally, the claim is submitted for reimbursement with all relevant supporting documentation.
The third stage is when payer management activities are essential to maximizing reimbursement by ensuring claim submissions include prior authorizations, clinical documentation, proprietary payer forms and comply with payer policies and requirements. Through this stage, patient engagement ensures all the correct data is in place, and insurance information or coverage hasn’t changed or is appropriately updated. Anticipating payer responses and subsequent actions is critical to collecting the full amount payers are responsible for to minimize patient financial impact. Once all payer activities are exhausted, the patient must be sent their statement for the remaining balance in their preferred communication method (paper, text, email, portal, etc.). Additionally, payment collection is accelerated when a diagnostic provider makes it easy and convenient to make payments, manage payment plans, and change payment methods.
These three stages in the patient journey encompass important revenue levers that cannot be overlooked. They are foundational to automating the financial performance engine needed for molecular diagnostics and pathology practices, Blattner continued. Whereas specialty diagnostics are rapidly coming to market and localized with varying reach, availability, and insurance coverage assurance, activating specific “clearance” functions or “engagement” opportunities within these levers will be key to smooth claims processing, timely filing, and optimizing all payment avenues.
Blattner stresses that when not built into automatic administrative functions, these three types of stages (i.e., patient access, physician engagement, and payer management) will slow or indefinitely stall payment for molecular diagnostics and pathology providers.
Market Expansion and Shift in at-Home Testing Stresses Traditional Administrative Approaches
Novel diagnostics are being introduced in record numbers as physicians and diagnostic business leaders seek to address and fulfill unmet diagnostic and medical needs to support better health outcomes. Along with these new medical breakthroughs comes the demand for traditional administrative approaches to reinvent themselves – including RCM. This major operational shift and frequent payer policy changes with advanced diagnostics have strained traditional administrative practices. According to Blattner, when executives realize that manual processes and inadequate electronic billing functions have reached a breaking point, specialized automation is the natural next step. The items corresponding to the highest value revenue cycle activities may sound surprising within the three revenue levers—patient access, medical clearance, and payer management.
Patient Access, Engagement, and Financial Clearance
“Making it easy for physicians to order molecular diagnostics and pathology tests is so important for success in today’s market,” Blattner continued. Ordering physicians and lab teams must have accurate and timely information regarding a patient’s ‘financial clearance’ (the likelihood a test will be covered, what the patient is likely to be charged out-of-pocket, and whether prior authorization is required). Patient portals and multi-channel communications are important parts of effective RCM functionality that facilitate patient access and financial clearance.
“It used to be that a patient went to the lab, and a phlebotomist saw the patient, but now more tests involve specimen collection at home. A kit is distributed at the physician’s office or ordered online and shipped to the patient,” Blattner said. “There is more follow-through needed to make sure not only did the test get done, but did it get returned, because while there are upfront costs to serve the patient, the lab doesn’t get paid until the test is completed, returned, processed and the diagnosis is determined for the claim to be processed. That is an evolution as these tests leave the laboratory or the business and enter the home environment.”
Patient access and engagement tools provide various benefits, including offering a cost-effective alternative to traditional customer service calls and supporting patients’ communication preferences. Effective physician access and engagement programs and technology help diagnostic providers offer self-service tools that enable patients to securely log in, anytime, to:
- View statements
- Make credit card payments
- Set up payment plans (using lab-specified rules and parameters)
- Establish paperless billing
- View patient responsibility estimates
- View test results
Another critical aspect of patient financial clearance for diagnostic testing is the ability to provide patients with an accurate estimation of their out-of-pocket costs associated with a test. Practical patient communication tools enable ordering physicians’ staff members to assist patients in preparing for out-of-pocket expenses, which increases test completion rates and has been proven to reduce write-offs.
To accurately assess a patient’s financial responsibility, the estimation tool must consider relevant provider and plan specific pricing and test or procedure information, as well as provide access to real-time eligibility data. A proper estimation of a patient’s out-of-pocket expenses is also predicated on receiving complete and accurate information from the payer. Examining payer behavior can uncover responses that create inaccurate patient responsibility estimates.
Physician Engagement Programs Facilitate Clinical Clearance
Physician engagement programs help diagnostic providers integrate communication and data exchange more deeply with ordering physicians and complete clinical clearance. Clinical clearance involves things like medical necessity, familial history, and social determinants of health. Robust RCM also requires diagnostic providers, laboratories, and pathology practices to be able to seamlessly communicate with patients to ensure that samples, devices, or readings are collected and returned to the diagnostic provider so that services/tests can be completed.
Effective physician engagement and clinical clearance increase ordering volume, maximize clean claims and automate denials and appeals management. Physician engagement technology, including electronic communication tools such as portals, helps physicians and their teams streamline the online correction of missing information and errors. This improves satisfaction, expedites reimbursement, and provides cost savings. With effective physician engagement programs and technology tools, physicians and their staff can more effectively:
- Perform order entry
- Access clinical decision support
- Examine statements at the line-item level
- View test information and pricing
- Correct billing errors upfront to expedite reimbursement
- Provide patients with an estimate of their out-of-pocket cost
Payer Management
Molecular diagnostic and genetic tests are famously complex and present many unique operational and financial challenges for laboratories. Payer policies and behavior are constantly changing, and labs (and their billing partners) must stay abreast of changes to avoid lengthy delays that denials and subsequent appeals can cause. Intelligent automation of prior authorizations, insurance discovery, and benefits determination are especially important for these tests.
Unfortunately, it is common for diagnostic providers to only learn about a change in reimbursement after the month-end close. These changes manifest in billing as:
- New denials
- Changes in denial rate
- Changes in reimbursement rate
- Change in time to payment
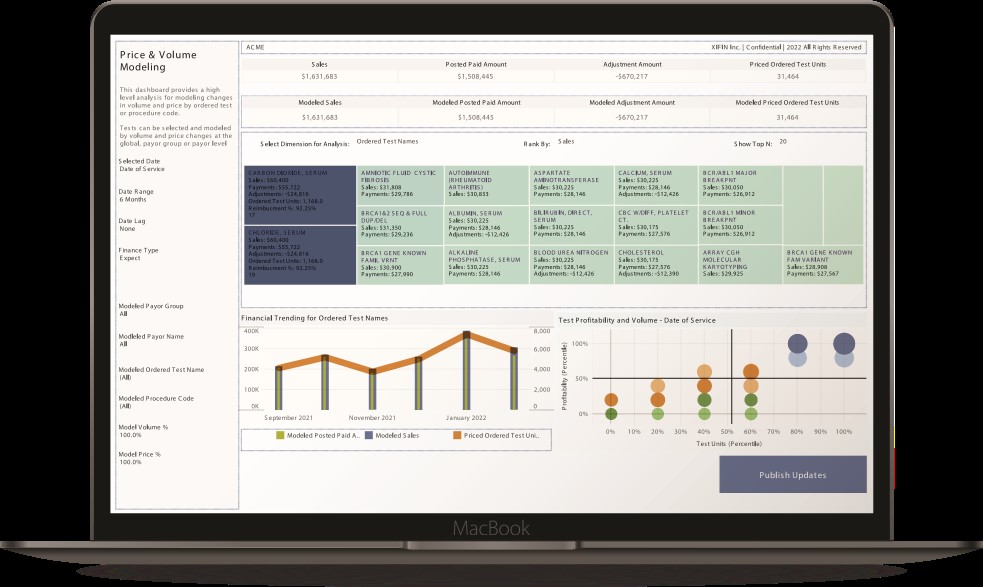
Failure to quickly recognize and adapt workflows to payer reimbursement changes can result in costly appeals and write-offs. XiFin recommends that providers adopt a proactive strategy to identify changes in reimbursement earlier. It is essential to understand the impacts and risks of price discrepancies and changes in pricing to patients. Staying abreast of policy changes for Medicare and commercial payers enables molecular diagnostic laboratories and pathology groups to proactively employ front-end billing system edits to avoid denials.
Keys to Success
For molecular diagnostic providers and pathology groups to maximize reimbursement, CFOs, and revenue cycle leaders must take a broader view of RCM. The RCM process starts well before billing and runs parallel to the patient journey in many respects. This means that effective RCM technology and tools also stretch beyond the billing system to incorporate seamless communication between systems and parties throughout the patient journey.
Adaptive RCM approaches require automation, intelligence, and real-time communication for the three key revenue-impacting stages discussed in this article: patient access, medical clearance, and payer management. This involves seamless integration with various tools that enable insurance discovery, patent demographic and eligibility verifications, patient financial responsibility estimation, and reporting and analytics that allow early identification of and response to changes in payer behavior.
Molecular diagnostic labs and pathology practices must have tools and technology to align with payers on evidence requirements, including clinical utility evidence, current billing policies, and preferred coding approaches. They must have seamless connectivity to ordering physicians to order tests and ensure the completeness of medical necessity and medical record documentation.
Finally, XiFin recommends that diagnostic organizations use analytics to enable early insight into changes in payer behavior, address root causes, and be able to adjust to changes in ordering patterns and client data quality. Be sure to consider an RCM platform that has embedded artificial intelligence (AI) to drive efficient automation of workflow adaptation to payer changes and future-proof your RCM investment.
Financial executives seeking to maximize market access and capitalize on growth opportunities in key markets will want to explore how successfully their administrative teams are navigating the unique revenue cycle landscape specific to molecular testing and pathology.
Part 2 of this three-part series is coming soon. Watch for updates here at DarkDaily.
— Leslie Williams


