UCSF Researchers Discover COVID-19 Coronavirus Evolved to Grow Tentacles and Use Them to Infect Other Cells!
Study scientists identified several currently available drugs that could inhibit growth of these “streaming filaments,” which infected cells use to go after non-infected cells
Like a scene from a bad horror movie, scientists have discovered that SARS-CoV-2, the coronavirus responsible for the COVID-19 pandemic, may be even more sinister and macabre than previously thought. The new research findings will interest those pathologists and clinical laboratory professionals who want to understand how the coronavirus spreads once it enters the body.
Headed by scientists from the University of San Francisco (UCSF), a team of international researchers discovered that “when the SARS-CoV-2 virus infects a human cell, it sets off a ghoulish transformation,” reported the Los Angeles Times (LA Times).
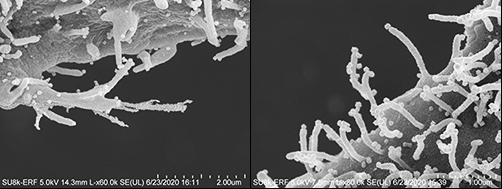
“Obeying instructions from the virus,” the LA Times continued, “the newly infected cell sprouts multi-pronged tentacles studded with viral particles. These disfigured zombie cells appear to be using those streaming filaments, or filopodia, to reach still-healthy neighboring cells. The protuberances appear to bore into the cells’ bodies and inject their viral venom directly into those cells’ genetic command centers—thus creating another zombie.”
As If the Coronavirus Weren’t Bad Enough!
“It’s just so sinister that the virus uses other mechanisms to infect other cells before it kills the cell,” Nevan Krogan, PhD, Professor, Department of Cellular Molecular Pharmacology at the UCSF School of Medicine, one of the study’s authors, told the LA Times.
The researchers published their study, titled, “The Global Phosphorylation Landscape of SARS-CoV-2 Infection,” in the journal Cell.
SARS-CoV-2 Has Evolved, Study Suggests
Prior to this discovery, scientists believed that the coronavirus infected cells in a typical fashion by finding receptors on the surface of cells lining an individual’s mouth, nose, respiratory tract, lungs or blood vessels, and eventually replicating and invading larger cells. However, this new research may suggest that the virus has evolved and developed new ways to pass quickly and effectively from cell to cell.
While some other illnesses, including smallpox, human immunodeficiency virus (HIV), and some influenza viruses have been known to use filopodia to enhance their ability to infect cells, Krogan contends that those other viruses do not seem to have the prolific growth of the SARS-CoV-2 filopodia.
“By conducting a systematic analysis of the changes in phosphorylation when SARS-CoV-2 infects a cell, we identified several key factors that will inform not only the next areas of biological study, but also treatments that may be repurposed to treat patients with COVID-19,” he said, in a UCSF news release.
UCSF Study Identifies Drugs, Compounds That May Disrupt Growth of Filopodia
One key finding is that the coronavirus was utilizing a specific type of molecule from a family of cellular helpers known as Kinase to create the filopodia.
The researchers conducted a “quantitative mass spectrometry-based phosphoproteomics survey of SARS-CoV-2 infection in Vero E6 cells,” the study noted, which revealed a “dramatic rewiring of phosphorylation on host and viral proteins.
“SARS-CoV-2 infection promoted casein kinase 2 (CK2) and p38 MAPK activation, production of diverse cytokines, and shutdown of mitotic kinases, resulting in cell cycle arrest,” the study continued, adding, “Infection also stimulated a marked induction of CK2-containing filopodial protrusions possessing budding viral particles.
“Eighty-seven drugs and compounds were identified by mapping global phosphorylation profiles to dysregulated kinases and pathways. We found pharmacologic inhibition of the p38, CK2, CDK, AXL, and PIKFYVE kinases to possess antiviral efficacy, representing potential COVID-19 therapies,” the researchers concluded.
To determine if they might be helpful in combating COVID-19, the UCSF research team tested drugs and compounds that were either already cleared to market by the US federal Food and Drug Administration (FDA), in clinical trials, or under preclinical development.
After discovering the Kinase connection, the scientists focused on specialized drugs known as Kinase inhibitors.
“We narrowed in on about a dozen, and we highlighted about six or seven that look particularly potent in a laboratory setting,” Krogan told ABC News. “And we’re very excited now to try and take these into clinical trials.”
Among the drugs the study identified as potentially being able to disrupt the creation of filopodia and slow the spread of COVID-19 in the body are:
- Silmitasertib: A drug that is currently in the clinical trial stages as a treatment for bile duct cancer and other cancers, including hematological and lymphoid malignancies;
- Ralimetinib: An experimental cancer drug; and
- Gilteritinib: A drug used to treat acute myeloid leukemia.
“We are encouraged by our findings that drugs targeting differentially phosphorylated proteins inhibited SARS-CoV-2 infection in cell culture,” said Kevan Shokat, PhD, Professor of Cellular and Molecular Pharmacology at UCSF, and co-author of the study, in the UCSF news release. “We expect to build upon this work by testing many other kinase inhibitors, while concurrently conducting experiments with other technologies to identify underlying pathways and additional potential therapeutics that may intervene in COVID-19 effectively.”
Presently, the UCSF study provides no direct benefit to COVID-19 illness patients or clinical laboratories performing SARS-CoV-2 testing. However, that could change rapidly. Pathologists and medical laboratory managers will want to keep an eye on this research, because it may lead to new treatments for COVID-19 that would require increased clinical laboratory testing to identify people infected with the coronavirus.
—JP Schlingman
Related Information:
Inside the Body, the Coronavirus is Even More Sinister than Scientists had Realized
The Global Phosphorylation Landscape of SARS-CoV-2 Infection
Coronavirus Hijacks Cells, Forces them to Grow Tentacles, then Invades Others
UCSF Researchers Look to Turn COVID-19’s Weapons Against Itself



