Nov 28, 2018 | Digital Pathology, Instruments & Equipment, Laboratory Instruments & Laboratory Equipment, Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing
Clinical laboratory leaders aiming for patient-centered care and precision medicine outcomes need to acknowledge that patients do not want to be in hospitals or travel to physician offices and patient care centers for blood tests. It can be inconvenient, sometimes costly, and often painful.
That’s why disease management methods such as remote patient monitoring are appealing to many people. It’s a big market estimated to reach $1 billion by 2020, according to a Transparency Market Research Report. The study also associated popularity of devices such as heart rate and respiratory rate monitors with economic pressures of unnecessary hospital readmissions.
But can remote patient monitoring be used for more than to check heart rates, monitor blood glucose, and track activity levels? Could such technology be effectively leveraged by medical laboratories for remote blood sampling?
Microsampling versus Dried Blood Collecting
Remote patient monitoring must be able to address a large number of diseases and chronic health conditions for it to continue to expand and gain acceptance as a viable way to care for patients in different settings outside of hospitals. However, as most clinical pathologists and laboratory scientists know, clinical laboratory testing has an essential role in patient monitoring. Thus, there is the need for a way to collect blood and other relevant samples from patients in these remote settings.
One promising approach is the development of new microsampling technology that can overcome past obstacles of dried blood collection. Furthermore, microsampling-enabled devices can make it possible for medical laboratories to reach out to the homebound to secure accurate and volumetrically appropriate samples in a cost-effective manner.
“One well-established fact in today’s healthcare system is that an ever-greater proportion of patients want clinical care that is less invasive and less intrusive,” noted Robert Michel, Editor-in-Chief of Dark Daily and The Dark Report. “Patients want to take more control over their treatment and be more effective at maintaining the stability of their chronic conditions, and often are happier than those who need to travel to have chronic conditions monitored. To meet this need there has been significant innovation, particularly in the area of remote blood sampling using microsampling technology.”
For decades, medical laboratories have tried various methods for acquiring and transporting blood samples from remote locations. One such non-invasive alternative to venipuncture is called dried blood spot (DBS) collecting. It involves placing a fingerprick of blood on filter paper and allowing it to dry prior to transport to the lab.
But DBS collected bio samples often do not contain enough hematocrit (volume percentage of red blood cells) for laboratories and clinical pathologists to provide accurate reports and interpretations. Reported reasons DBS cards have not penetrated a wide market include:
- Hematocrit bias or effect;
- Costly card punching and automation equipment; and,
- Possible disruption to existing lab workflows.
Microsampling Technology Enables Collection of Appropriate Samples
Microsampling has to have the capability to enable labs to deliver quality results from reliable blood samples. This remote sampling technology makes it possible for phlebotomists to offer a comfortable collection alternative for homebound patients and rural residents. It also can be useful for physicians stationed in remote areas. Patients themselves can even collect their own blood samples.
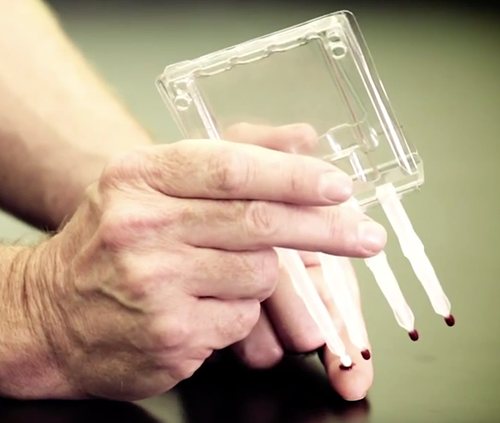
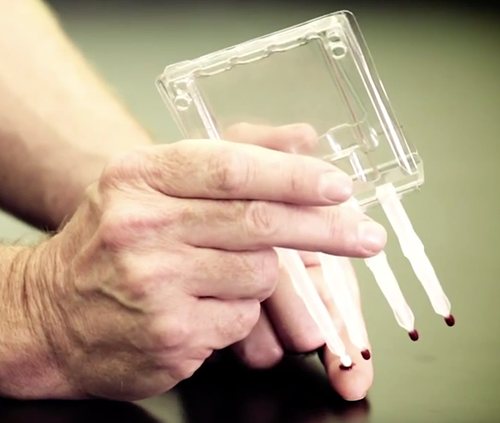
Volumetric Absorptive Microsampling (VAMS) technology enables accurate samples of blood or other fluids from amounts as small as 10, 20, or 30 microliters, according to Neoteryx, LLC, of Torrance, Calif., the developer of VAMS. The technology is integrated into the company’s Mitra microsampler blood collection devices (shown above) in formats for patient use and for medical laboratory microsample accessioning and extraction. Click here to watch a video on the Mitra Microsampler Specimen Collection Device. (Photo copyright: Neoteryx.)
One company developing these types of products is Neoteryx, LLC, of Torrance, Calif. It develops, manufactures, and distributes microsampling products. Patients with the company’s Mitra device use a lancet to puncture their skin and draw a small amount of blood, collect it on the device’s absorptive tip, and then mail the samples to a blood lab for testing (Neoteryx does not perform testing).

“Technologies such VAMS are driving [precision medicine] in an extremely cost-effective manner, while only requiring minimal patient effort. Patients are taking a more active role in their healthcare journeys, and at-home sampling is supporting this shift,” stated Fasha Mahjoor, Chief Executive Officer, Neoteryx, in a blog post. (Photo copyright: Neoteryx.)
Patient satisfaction survey data collected by Neoteryx suggest patients are comfortable with their role in blood collection:
- 70% are comfortable or very comfortable with the process;
- 86% say it is easy or very easy to use the Mitra device;
- 92% report it is easy to capture blood on the device’s tip;
- 55% of Mitra device users are likely or very likely to choose microsampling over traditional venipuncture; and,
- 93% noted they are likely or very likely to choose the device for child care.
A list of published studies describes certain advantages of VAMS technology that have implications for medical laboratories and clinical pathologists:
- Microsampling has benefits and implications for therapeutic drug monitoring, infectious disease research, and remote specimen collection;
- Dried blood microsamples from fingerstick can generate reliable data “correlating” to traditional blood collection processes;
- Bioanalytical data collected with the Mitra device are accurate and dependable; and,
- In a study for a panel of anti-epileptic drugs, VAMS led to optimized extraction efficiency above 86%, which means there was no hematocrit bias.
Learn More by Requesting the Dark Daily Microsampling White Paper
To help medical laboratories and clinical pathologists learn more about microsampling and VAMS devices, Dark Daily and The Dark Report have produced a white paper titled “How to Create a Patient-Centered Lab with Breakthrough Blood Collection Technology: Microsampling Takes Blood Collection Out of the Clinic.” The paper includes sections addressing these topics:
- Rise of patient-centered care and remote patient monitoring;
- Dried blood collection over the years and the hematocrit effect;
- A look at microsampling and how it takes blood collection out of the clinic;
- How Volumetric Absorptive Microsampling (VAMS) technology works;
- Patient satisfaction data;
- Research about microsampling including extensive graphics;
- Launching new VAMS technology; and,
- Frequently asked questions.
Innovative medical laboratory leaders who want to increase their understanding of how microsampling technology and remote patient monitoring relates to the goal of becoming a patient-centered lab are encouraged to request a copy of the white paper. It can be downloaded at no cost by clicking here, or placing https://www.darkdaily.com/how-to-create-a-patient-centered-lab-with-breakthrough-blood-collection-technology-9-2018/ into your browser.
—Donna Marie Pocius
Related Information:
Remote Patient Monitoring Devices Market
Neoteryx, LLC, and Cedars Sinai Partner to Investigate at Home Blood Sampling Possibilities for Patients with Inflammatory Bowel Disease
Creating a Patient-Centered Lab with Breakthrough Blood Collection Technology Using New Microsampling Methods Provides Reliable, Economic Collection, Shipping and Storage Solutions
How to Create a Patient-Centered Lab with Breakthrough Blood Collection Technology: Microscopy Takes Blood Collection Out of the Clinic
Nov 27, 2017 | Laboratory Management and Operations, Laboratory News, Laboratory Operations, Laboratory Pathology, Laboratory Testing, Management & Operations, News From Dark Daily
November workshop to teach Clinical Lab 2.0 to forward-thinkers among clinical laboratories, IVD manufacturers, and lab IT vendors offered many examples where clinical laboratory diagnostics can add value and improve patient outcomes
DATELINE: ALBUQUERQUE, New Mexico—Here in this mile-high city, a special Project Santa Fe Workshop devoted to teaching the principles of Clinical Lab 2.0 attracted an impressive roster of innovators and forward-thinkers in clinical laboratory medicine. In attendance were leaders from a select number of the nation’s first-rank health systems and hospitals, along with executives from In Vitro diagnostics (IVD) manufacturers, lab IT companies, other lab service companies, attendees from the Centers for Disease Control and Prevention, and from institutions in Canada, Germany, Israel, India, and the UK.
Their common goal was to learn more about the emerging clinical and business model for medical laboratories known as “Clinical Lab 2.0.” A key objective of the workshop was to help those lab leaders in attendance develop strategic action plans for their own lab organizations, so as to take advantage of the insights coming from the vast information streams generated by their clinical laboratories. These services would be in support the evolving needs of health systems, hospitals physicians, and health insurers to more effectively provide integrated patient-centered clinical care.
Medical Laboratories Can Use Clinical Lab 2.0 as a Path to Adding Value
Clinical Lab 2.0 is the clinical and business model of the future for medical laboratories, assert the developers of this concept. “Clinical Lab 2.0 describes the attributes needed by all medical laboratories that want to succeed in a healthcare system organized to provide precision medicine, keep people out of hospitals, and where providers—including labs—are reimbursed based on the value they provide,” stated Khosrow Shotorbani, CEO of TriCore Reference Laboratories, one of the organizers of the Project Santa Fe Clinical Lab 2.0 Workshop.
“Clinical Lab 2.0 is the path medical labs will need to follow if they are to continue providing relevant lab testing services and generate the reimbursement necessary for them to maintain a high level of clinical excellence and financial stability going forward,” he added. “This is the next generation of medical laboratory organization and operation.”
Lab 1.0 Was Lab Clinical/Business Model for 50 Years
For more than 50 years, Clinical Lab 1.0 was the model for labs,” noted James Crawford, MD, PhD, Executive Director and Senior Vice President of Laboratory Services at Northwell Health Laboratories and an organizer of the Project Santa Fe Clinical Lab 2.0 Workshop. “Lab 1.0 is transactional, focusing on generating high quality analytical data on specimens received, but without assembling these data into integrative clinical care programs. In the simplest sense, Clinical Lab 1.0 focused on generating ever-greater numbers of specimens to drive down average cost-per-test, while maximizing revenue in a fee-for-service system.

This chart shows the attributes of Clinical Lab 1.0 and compares those to the attributes of Clinical Lab 2.0. Lab 1.0 is transactional and based on increasing test volume to lower costs and maximize fee-for-service revenue. Clinical Lab 2.0 is integrative in ways that add value to lab testing services. (Graphic copyright Project Santa Fe.)
“But fee-for-service payment is going away,” he said. “Increasingly, clinical laboratories will be paid based on the value they provide. This payment can be in the form of bundled reimbursement, as a per-member-per-month payment, or as a share of the budgeted payment made to a health system, an accountable care organization (ACO), or a multispecialty provider network. As these alternative forms of provider payment become dominant, to earn a fair share of reimbursement, all medical laboratories will need a clinical strategy to deliver lab testing services that measurably contribute to improved patient outcomes while reducing the overall cost of care. This requires looking at medical laboratories’ contribution to effective delivery of the full dollar of the healthcare spend, not just the three-cents-on-the-dollar representing laboratory testing.”
Innovators in Clinical Laboratory Industry Identify New Ways to Add Value
There are already a handful of innovative clinical laboratory organizations that have clinical experience in moving past the Lab 1.0 paradigm of reporting an accurate test result within the accepted turnaround time. Leaders within these labs are collaborating with physicians and frontline care givers specifically to help them better utilize lab tests in ways that directly improve the speed and accuracy of the overall diagnostic sequence, as well as achieving therapeutic optimization as rapidly as possible. These collaborations are tracking the improvement in patient outcomes while demonstrating how better use of lab tests can lower the total cost per episode of care.
During the Clinical Lab 2.0 workshop, case studies were presented demonstrating how clinical laboratory leaders are taking the first steps to practice Clinical Lab 2.0 so as to achieve added value with medical laboratory tests. The case studies included:
· A project to improve diagnosis and treatment of sepsis at Geisinger Health System.
· A project at Henry Ford Health to collaborate with physicians to more appropriately utilize lab tests and build consensus in support of a new lab test formulary.
· A multi-hospital initiative at Northwell Health to collaborate with physicians and nurses in the use of creating testing to make earlier, more accurate diagnoses of acute kidney injury during inpatient admissions, and better guide decisions to treat.
· A partnership involving TriCore Reference Laboratory and certain health insurers in New Mexico where the laboratory—using lab test data (some generated by emergency room testing) and other clinical data—alerts the insurers to women who are pregnant, thus allowing the insurers to provide timely guidance to the women’s care teams with the goal of improving prenatal care.

The Project Santa Fe Clinical Lab 2.0 Workshop convened on November 13-14 in Albuquerque, N.M. A broad spectrum of innovative professionals from the five Project Santa Fe member laboratories (above) were there to teach the lessons learned from their first successful efforts to collaborate with physicians and create added value from medical laboratory diagnostics. Other attendees included progressive lab leaders from several of the nation’s most prominent health systems, along with thought leaders from the IVD, lab software, and lab association sectors. (Photo copyright Project Santa Fe.)
Project Santa Fe Workshop: A Well-Attended Lab ‘Think Tank’
Participants attending the Clinical Lab 2.0 workshop included hospital lab administrators, pathologists, and clinical laboratory industry executives. The importance of this workshop is reflected in the educational grants and financial support provided by leading in vitro diagnostics manufacturers, lab IT companies, and other lab industry vendors. The lab industry vendors included:
· Abbott Laboratories
· ARUP Laboratories
· Beckman Coulter
· DiaSorin
· MedSpeed
· Roche Diagnostics
· Siemens Healthineers
· Sysmex
Also providing educational grants and similar support were:
· American Clinical Laboratory Association
· CAP Today
· Centers for Disease Control and Prevention
· Mayo Medical Laboratories
· The Dark Report
Project Santa Fe was launched in 2016 by clinical lab leaders from five of the nation’s most respected integrated health systems:
· TriCore Reference Laboratories;
· Henry Ford Health;
· Geisinger Health;
· Kaiser Permanente Northern California; and,
· Northwell Health.
Described as a think-tank venture, the organizers are committed to implementing projects that demonstrate how lab tests can be used in ways that add value, and then publish the resulting projects, along with data about improved patient outcomes and reductions in healthcare costs, in peer-reviewed journals. Multi-institutional studies will be required to validate the findings and outcomes from the added-value clinical collaborations initiated at the different medical laboratory organizations participating in Project Santa Fe.
Another primary goal is to share the lessons learned from these innovative projects with other like-minded pathologists, lab administrators, and lab managers. In May, Project Santa Fe organizers led a one-day workshop to teach Clinical Lab 2.0 at the Executive War College on Laboratory and Pathology Management. The workshop in Albuquerque on November 13-14 was the second learning opportunity available to medical laboratory professionals. A November 2018 workshop is planned.
—Robert L. Michel
Related Information:
Project Santa Fe Workshop
Improving American Healthcare through “Clinical Lab 2.0”: A Project Santa Fe Report
Laboratory 2.0: Changing the Conversation
CEO Describes Characteristics of the Clinical Lab 2.0 Model: Five Health System Labs Using Project Santa Fe To Demonstrate Value
Moving to Clinical Lab 2.0: Deliver More Value! Get Paid More Dollars!
Lab Innovators Advocate Need for Clinical Lab 2.0: Lab 1.0 Is the Low-Paid Commodity Lab, While Lab 2.0 Gets Paid More for the Value It Contributes
Using the Laboratory Value Pyramid and Clinical Lab 2.0 to Position Your Lab to Add Value in the Era of Population Health, Precision Medicine, and Value-Based Payment