The U.S. Air Force Research Laboratory tapped nanotechnology experts at the University of Massachusetts Amherst to develop a patch that targets stress biomarkers in sweat
One potential disruptor of medical laboratory testing, as it exists today, are wearable biometric devices. These are already popular with athletes and health-conscious people. To meet this demand, a continual stream of innovative biometric gear is hitting the marketplace.
Foremost among the consumers for this technology is the U.S. military. Military leaders recognize the importance of monitoring the physical condition and health of armed forces personnel in the field. Wearable biometric devices are a perfect solution to meet this need.
Wearable Biometric Devices Could Perform Clinical Laboratory Tests
Ongoing improvements to this technology has motivated the U.S. military to develop its own version of a wearable device to monitor stress and fatigue in armed forces personnel, whose missions put them in stressful situations. What will interest clinical laboratory managers and pathologists is that this wearable device will monitor chemicals in sweat that are that indicators of stress and fatigue, according to a press release issued by the Nano-Bio Manufacturing Consortium (NBMC), an industry organization backed by the U.S. Air Force Research Laboratory (AFRL) and industry partners.
NBMC has awarded the University of Massachusetts Amherst (UMass) a $450,000 grant to develop a wearable biometric patch that monitors certain biomarkers in sweat. This five-year project includes research contributions by the University of Cincinnati, and is also receiving research support from a collaboration of the AFRL and Nanostructures and Surfaces Laboratory NSLGE in the research arm General Electric Co. (NYSE: GE).
Stress and Fatigue Can Affect Command Decisions by Military Personnel
“Any time you’ve got someone making a command decision, you want to make sure they’re in the right frame of mind, that they’re alert, that they’re well rested,” stated James Watkins, Ph.D., a Umass Professor who is leading this project. He was quoted in a report published by the Boston Globe. Watkins is Director of the Center for Hierarchical Manufacturing-NSF Nanoscale Science and Engineering Center, (CHM).

Leading the research project to develop a useful biosensor that could be worn by military personnel to measure levels of stress and fatigue is James Watkins, Ph.D. (pictured above). He is Director of the Center for Hierarchical Manufacturing at the NSF Nanoscale Science and Engineering Center that is part of the University of Massachusetts Amherst. (Photo copyright University of Massachusetts Amherst.)
Obviously, military personnel in combat situations experience tremendous stress, but so do those that support them, noted Wayne Chappelle, Ph.D., Chief of Aeromedical Clinical Psychology at the Air Force School of Aerospace Medicine.
Cyber-warfare operators, such as drone pilots, for example, are susceptible to long-term stress that may affect performance, because they are often called upon to provide support for ground troops and witness injuries and deaths of their colleagues.
A paper by Chappelle and colleagues reported the results of a study that assessed symptoms of stress and fatigue in drone pilots. The study, which was published in the May 2014 issue of the Journal of Anxiety Disorders, found that more than 30% of the 1,084 drone pilots surveyed experienced symptoms of high chronic stress, such as difficulty sleeping, and nearly 15% of them reported having difficulty concentrating and/or suffered outbursts of irritability.
Biometric Patch to Detect Chemical Indicators of Stress in Sweat
“Biosensors are of significant interest to the Air Force due to their exceptional sensitivity for a wide variety of molecules and biomarkers, including Orexin-A, which is the focus of the NBMC project led by UMass,” noted Benjamin J. Leever, Ph.D., Program Manager for Flexible Materials and Devices and Research Engineer at AFRL, in the NBMC press release.
The UMass project calls for creating an inexpensive, disposable patch that contains elements that test chemicals in sweat. The patch’s electronic structures will to fit into a Band-Aid-size device and will not interfere with the patch’s flexibility.
Nanoscale Printing Technology Could Produce Patch for Under $1
The patch will act like a tiny computer, collecting sweat and extracting its chemicals via microscopic-gated channels. Electronics on the patch would then measure and wirelessly transmit the data for analysis by a medical professional. It will be constructed with tiny plastic elements, using roll-to-roll printing technology that inexpensively prints structures at a nanoscale, or molecular level, reported the Boston Globe.
“We want to be able to print these things for under a dollar,” declared Watkins. UMass has partnered with Carpe Diem, an innovative technology company in Franklin, to print the patches using a device developed by UMass scientists. The device prints at the 50-nanometer scale, which is 1,000 times smaller than a single human hair.
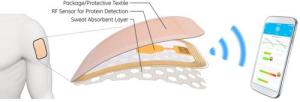
Above is an image of the patch under development at University of Massachusetts in Amherst in cooperation with four other universities, the U.S. Air Force Research Laboratory, and Nanostructures and Surfaces Laboratory at General Electric. The body has two types of sweat glands, eccrine and appocrine. It’s the appocrine glands—located in areas like the armpits and the groin—that are active during stressful situations and produce thicker, oil-like perspiration. Body odor comes from bacteria feasting on this kind of sweat. (Image copyright Val Gempis, U.S. Air Force.)
Three other universities also received funds from NBMC to conduct research and development projects that will be incorporated into the UMass project. These projects include developing electronics and biometric platforms for human-performance monitoring and assessing different methods and devices used to collect sweat under various conditions.
Military Supported Research Could Have Civilian Applications
“The military market is just one small piece of the market that exists,” observed Scott Miller, Ph.D., NSLGE Manager, in the Boston Globe article. “There’s the civilian market. It’s an extension of wearable electronics and fitness monitors.”
Jeffrey Morse, Ph.D., Managing Director of the National Nanomanufacturing Network and the UMass Center for Hierarchical Manufacturing, pointed out that many chemicals occurring in sweat also show up in blood. That means similar patches could be used to monitor heart rate and liver function. He also noted that succeeding generations of this patch could detect concussions and other indicators of health status. Furthermore, health patches could send data to a doctor wirelessly, eliminating the need for a blood test that is sent to a medical laboratory and the costs associated with such lab testing, Morse told the Boston Globe.
This research project will spur a larger push at UMass to build new nanotechnology infrastructure, suggested the Boston Globe report, noting that Watkins’ team received $46 million last year from the Massachusetts Life Sciences Center, a state-run initiative, to build a laboratory dedicated to creating personalized health monitors. UMass’ Center for Hierarchical Manufacturing also received $36 million from the National Science Foundation to fund research by the CHM.
Similar to products originally created by the National Aeronautics Space Agency (NASA), products created by the CHM will likely be adapted to needs of consumers. With substantial funding of this application of nanotechnology, scientists involved in this project expect this research to eventually produce wearable sensors that would allow pathologists and other physicians to monitor patients remotely in real time. If such a capability became reality, it would create a new opportunity for pathologists and clinical laboratory scientists to consult with physicians and be more involved in early diagnosis and decisions about appropriate therapies.
—by Patricia Kirk
Related Information:
UMass patch would spot stressed-out soldiers
Binghamton University for Development of Electronics and Biometric Sensor Platforms
An analysis of post-traumatic stress symptoms in United States Air Force drone operators
Meet the Fearbit: New Sweat Sensors Will Sniff Out Fatigue, Stress and Even Fear



