Clinical Pathology Laboratories Swamped With Requests to Interface Their LISs to EHRs
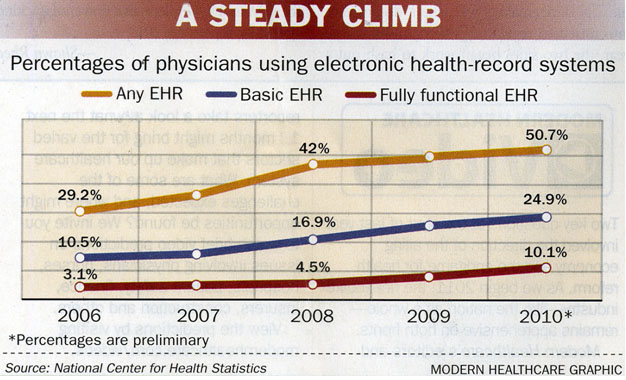
This is the first year that hospitals and physicians can qualify for federal incentives associated with their adoption and meaningful use of electronic health record (EHR) systems. Already clinical laboratories and pathology groups report increasing demand for them to interface their laboratory information systems (LIS) to the physicians’ EHRs.
The financial incentives for hospitals and physicians are authorized as part of the federal government’s health information technology (HIT) incentive program. To get their fair share, healthcare providers must demonstrate by the end of 2011 (September 30th for hospitals) a 90-day contiguous meaningful use of an electronic health record (EHR) for Medicare transactions—and either adopt, implement or upgrade an EHR for Medicaid also within 90 days. Hospitals can receive payments for both, but physicians only one.
(Sourced from Modern Healthcare.)
Published data says that hospitals and health systems have a long way to go before full adoption becomes a reality. Research by the Harvard School of Public Health (HSPH) titled “A Progress Report on Electronic Health Records in U.S. Hospitals,” recently published in Health Affairs, concluded that only 11.9% of hospitals in America operated either a basic or comprehensive EHR, and only 2% of them operated EHRs that would pass the Stimulus bill’s criteria for meaningful use, and therefore receive part of the $25.8 billion in HIT adoption incentive payments.
2011 sets the stage for a huge rush to adoption. Many clinical laboratories and anatomic pathology groups are swamped by requests from physician groups to provide an interface between the lab’s LIS and the client physician’s EHR.
EHR Adoption Problematic for Small and Rural Hospitals
Not only is the EHR adoption rate low among hospitals and health systems, according to the study, it’s even lower among small and rural hospitals. That’s primarily a result of two factors. One is the cost of implementing an EHR, which can run into the tens of millions of dollars. The other is the state of the economy in many rural areas. HSPH researchers are concerned that this disparity will continue to widen, and that when push comes to shove, only the larger academic hospitals will qualify for government incentive payments.

Ashish Jha, M.D., Associate Professor of Health Policy and Management at Harvard School of Public Health. (Sourced from HSPH website.)
“The problem is that the bonuses that hospitals get for meeting meaningful use are front-loaded, meaning hospitals have to implement and use EHRs by 2012 in order to get the bulk of the incentives,” said the study’s lead author Ashish Jha, M.D., Associate Professor of Health Policy and Management. “This is an aggressive timeline, and many hospitals may not make it. If they miss out, it may be years before many of these hospitals will be able to afford to purchase and install their own EHR systems.”
Meaningful Use Can Be Met with Medical Laboratory Test Ordering and Reporting
To receive payments, healthcare professionals must implement an EHR and use it continuously for Medicare and/or Medicaid patients for 90 days to prove meaningful use. Providers must also show that they participated in a meaningful electronic information exchange of patient health data. It is believed most providers will want electronic clinical laboratory test ordering and laboratory test reporting functions to be among the meaningful use criteria they use to meet the requirements for federal incentives.
Depending on the year they installed their EHR, physicians and other healthcare providers receive payments from the government as follows:
- Year One: Up to $18,000 if adopted in 2011/2012. $15,000 otherwise.
- Year Two: $12,000
- Year Three: $8,00
- Year Four: $4,000
- Year Five: $2,000
Feds Get Serious About IT Adoption
Ever since the passage of the American Reinvestment and Recovery Act (ARRA) in February of 2009, enthusiasm to implement EHRs by hospitals has been lackluster at best.
To help incentivize healthcare providers to adopt IT even further, the government is offering:
- Workforce development programs at all college levels
- Funding support for the development of HIT exchanges
- Regional HIT extension centers to help hospitals and physicians investigate and select EHR systems.
It’s not often that pathologists and clinical lab managers get an idea of exactly what the HIT user base is amongst physicians and hospitals. This will be a watershed year for HIT adoption. How this more broadly affects the U.S. healthcare system remains to be seen. However, because of the important role that medical laboratory testing plays in most healthcare activities, it is certain that clinical laboratories and pathology groups will be engaged in helping their parent hospitals and their client physicians achieve EHR adoption, then meeting the meaningful use criteria necessary for them to successfully receive federal incentive payments.
Related Information:
U.S. Hospitals Making Only Modest Gains in Adoption of Electronic Health Records
A Progress Report On Electronic Health Records In U.S. Hospitals


